Why the World Turns Pink Every October
Breast Cancer Awareness Month, known in France as “𝘖𝘤𝘵𝘰𝘣𝘳𝘦 𝘙𝘰𝘴𝘦,” is an annual international health campaign held every October, coordinated by leading breast cancer charities around the world. The campaign aims not only to raise public awareness about breast cancer but also to mobilize support for research into its causes, prevention strategies, and innovative treatments. It provides vital encouragement to patients, survivors, and their families, while reminding society that collective action can save lives.
Awareness is especially important because breast cancer is the most common cancer among women worldwide1;2. However despite its prevalence, the disease can often be subject to some misconceptions.
Breast Cancer: Myths vs Facts
Myth #1: All breast cancers are the same.
Fact #1: Breast cancer isn’t one disease. There are several types, each with different growth patterns, responses to treatment, and outcomes. Research now allows treatments to be personalized for each patient3;4.
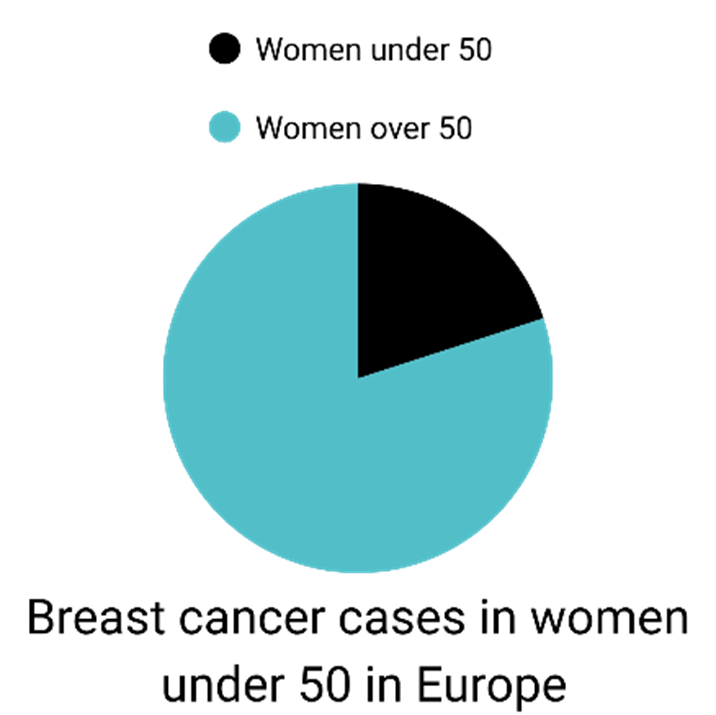
Myth #2: Breast cancer only affects middle-aged or older women.
Fact #2: Risk rises with age, but young women can also get breast cancer. Diagnoses in women under 50 are increasing, and younger patients often face more aggressive forms3;4;5.
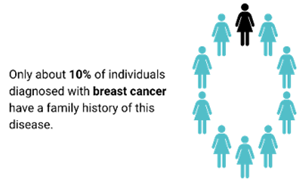
Myth #3: Most women with breast cancer have a family history or genetic mutation.
Fact #3: Only 10% of cases are due to inherited mutations. Most women diagnosed have no family history or known genetic mutation3;4.
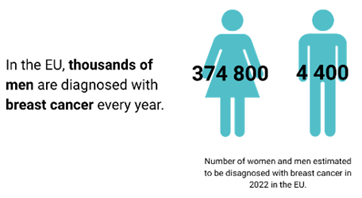
Myth 4: Only women can get breast cancer.
Fact 4: Men can get it too, representing around 1% of all cases. Thousands of men are diagnosed annually in the EU, often later and with worse outcomes due to lower awareness5.
Myth 5: Every breast lump is a sign of cancer.
Fact 5: Most lumps are not cancer. However, any new or persistent change in the breast should be checked. Breast cancer can also be detected through routine screening before any lump is felt3;4.
Understanding Breast Cancer
Everyone, regardless of sex, has breast tissue made up of fat, connective tissue, and lymph nodes that support immune function. In women, this tissue also contains milk-producing glands6. Breast cancer develops when a breast cell undergoes a mutation and begins to grow and divide uncontrollably to form a tumor 7.
Several factors determine the type of breast cancer, its prognosis, and the most appropriate treatment options6 :
- The tumor’s location
- The tumor’s level of invasiveness
- The molecular receptors present on the tumor cells
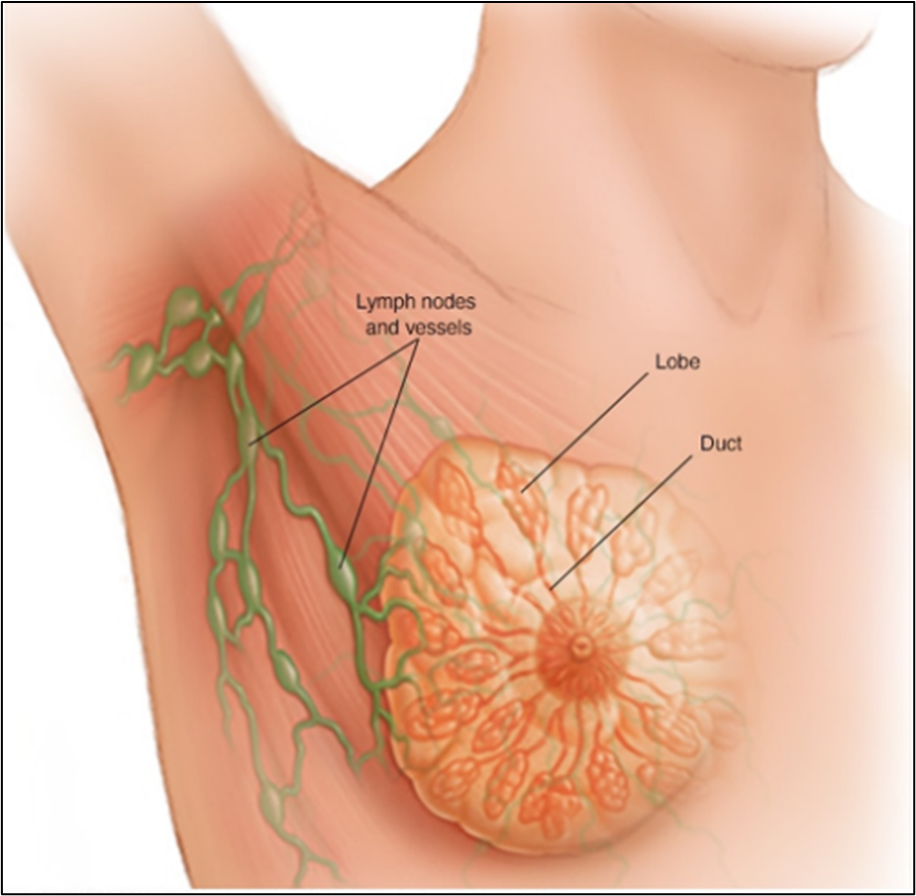
Common starting points of breast cancer tumors
Mayo Clinic. (2024). Breast cancer types: What your type means – Mayo Clinic.
Breast cancer symptoms can vary widely, and there’s no single way a lump or mass should feel. While self-exams are useful, many cancers are detected through routine mammograms before any symptoms appear6.
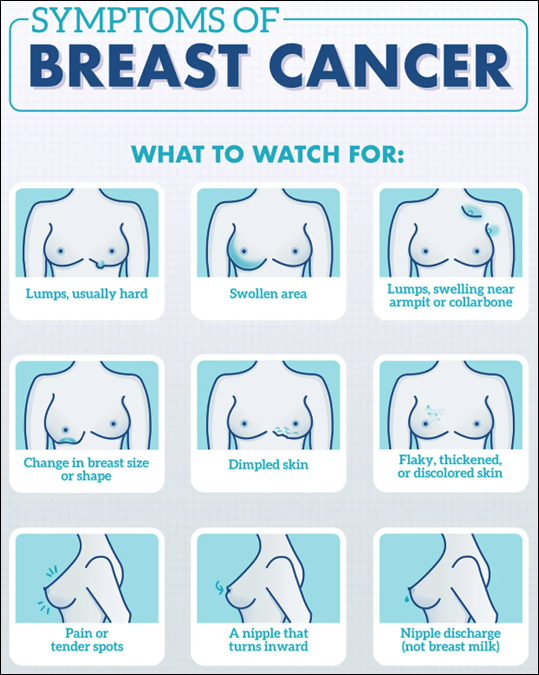
Most common breast cancer symptoms
WebMD (2024). Breast Cancer Symptoms and Early Warning Signs
The Impact of Breast Cancer
Breast cancer continues to have a profound global impact, as reflected in key statistics on its incidence and mortality. In fact, breast cancer is the most common cancer among women in 157 countries.
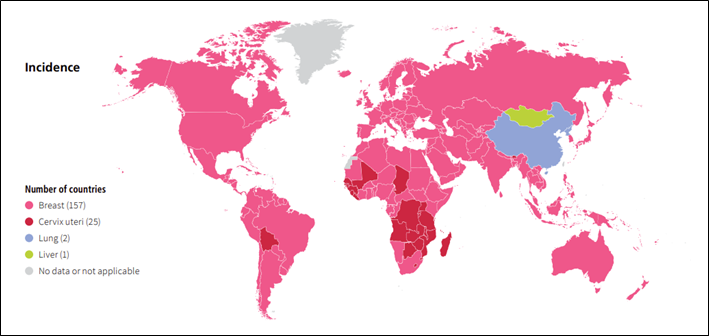
However, its impact extends beyond women, ranking as the second most common cancer overall worldwide, since men, though rarely, can also develop breast cancer8.
In addition to its high incidence, breast cancer represents the leading cause of cancer-related mortality in women, highlighting its significant impact on public health.
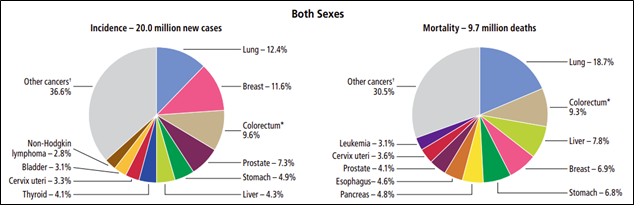
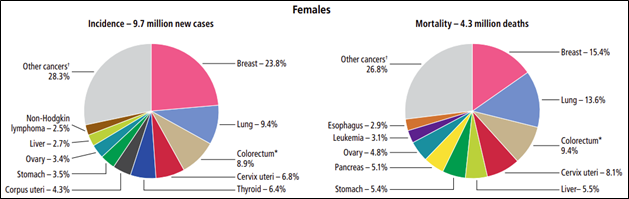
Distribution of cases and deaths for the 10 most common cancers
Global Cancer Facts & Figures-5th Edition
Thanks to early detection and major advancements in treatment, breast cancer mortality has declined over the past 25 years in North America and some regions of Europe9.
Nevertheless, global breast cancer incidence and mortality are expected to increase. Currently, 1 in 20 women worldwide will be diagnosed with breast cancer in their lifetime. If current trends persist, by 2050 there could be 3.2 million new cases and 1.1 million deaths from breast cancer each year10.
This further highlights the urgency of this issue, making early detection, education, and research more critical than ever. Preventing cancer is one of the biggest public health challenges of the 21st century. Research suggests that at least 40% of cases could be avoided through effective prevention strategies. For those who are diagnosed, about half will receive radiation therapy, a treatment that remains essential but still faces important limitations11.
THERYQ’s mission
At THERYQ, we are committed to pushing the boundaries of radiotherapy. Our focus is on FLASH radiotherapy, an innovative approach that delivers radiation to cancer cells in just a fraction of a second, while minimizing damage to surrounding healthy tissue12. By harnessing the potential of ultra-high dose-rate radiation, FLASH radiotherapy aims to shorten treatment times and reduce side effects, offering patients a safer and more tolerable option compared with conventional radiotherapy13. This approach represents a promising step forward in the fight against cancer, providing hope for patients who need better solutions today.
Disclaimer: FLASH radiotherapy is a novel technique, delivering radiation at ultra-high dose rates in a fraction of a second. This modality is currently being studied and is not clinically available.
Conclusion
Although breast cancer is widespread, important questions about its causes, progression, and optimal treatments remain unanswered, making it a persistent medical challenge. Its high incidence, biological complexity, and the therapeutic difficulties posed by aggressive subtypes keep it at the forefront of oncological research. Significant advances in screening, targeted therapies, and personalized medicine have greatly improved survival in recent decades, yet further progress is needed to reduce disparities in outcomes and improve long-term quality of life for all patients.
In the meantime, early detection remains our most effective defense, and by sharing awareness messages, we can all contribute to making a difference in the fight against breast cancer.
Sources
- American Cancer Society. (2024). Global cancer facts & figures (5th ed.). Global Cancer Facts & Figures-5th Edition
- World Cancer Research Fund. (2024). Breast cancer statistics. Breast cancer statistics | World Cancer Research Fund
- National Breast Cancer Foundation. (2023). Breast cancer myths & the truth behind the misconceptions. Breast Cancer Myths & The Truth Behind The Misconceptions
- Breast Cancer Research Foundation. (2023). Breast cancer myths debunked. Breast Cancer Myths Debunked | Breast Cancer Research Foundation
- Joint Research Centre. (2023, October). Breast cancer 2022 [PDF]. European Commission.pdf
- MD Anderson Cancer Center. (2024). Breast cancer. MD Breast Cancer – MD Anderson website
- World Health Organization. (2023). Breast cancer. Breast cancer WHO
- Jamil, A., Siddique, R., Altaf, F., Warraich, D., Ahmed, F., & Qureshi, Z. (2025). Comprehensive review of male breast cancer: Understanding a rare condition. Oncology research, 33(6), 1289–13 https://doi.org/10.32604/or.2025.058790
- Menon, G., Alkabban, F. M., & Ferguson, T. (2024). Breast Cancer. In StatPearls. StatPearls Publishing. Breast Cancer – StatPearls – NCBI Bookshelf
- World Health Organization – International Agency for Research on Cancer (2024). Breast cancer cases and deaths are projected to rise globally. Breast cancer cases and deaths are projected to rise global
- Lindner, J. (2025, May 1). Radiation therapy statistics: Market data report 2025. Worldmetrics. Radiation Therapy Statistics Statistics: Market Data Report 2025
- Panaino, C. M. V., Piccinini, S., Andreassi, M. G., Bandini, G., Borghini, A., Borgia, M., Di Naro, A., Labate, L. U., Maggiulli, E., Portaluri, M. G. A., et al. (2025). Very high-energy electron therapy toward clinical implementation. Cancers, 17(2), 181. https://doi.org/10.3390/cancers17020181
- Schüler, E., Acharya, M., Montay-Gruel, P., Loo, B. W., Vozenin, M., & Maxim, P. G. (2022). Ultra-high dose rate electron beams and the FLASH effect: From preclinical evidence to a new radiotherapy paradigm. Medical Physics, 49(3), 2082–2095. https://doi.org/10.1002/mp.15442