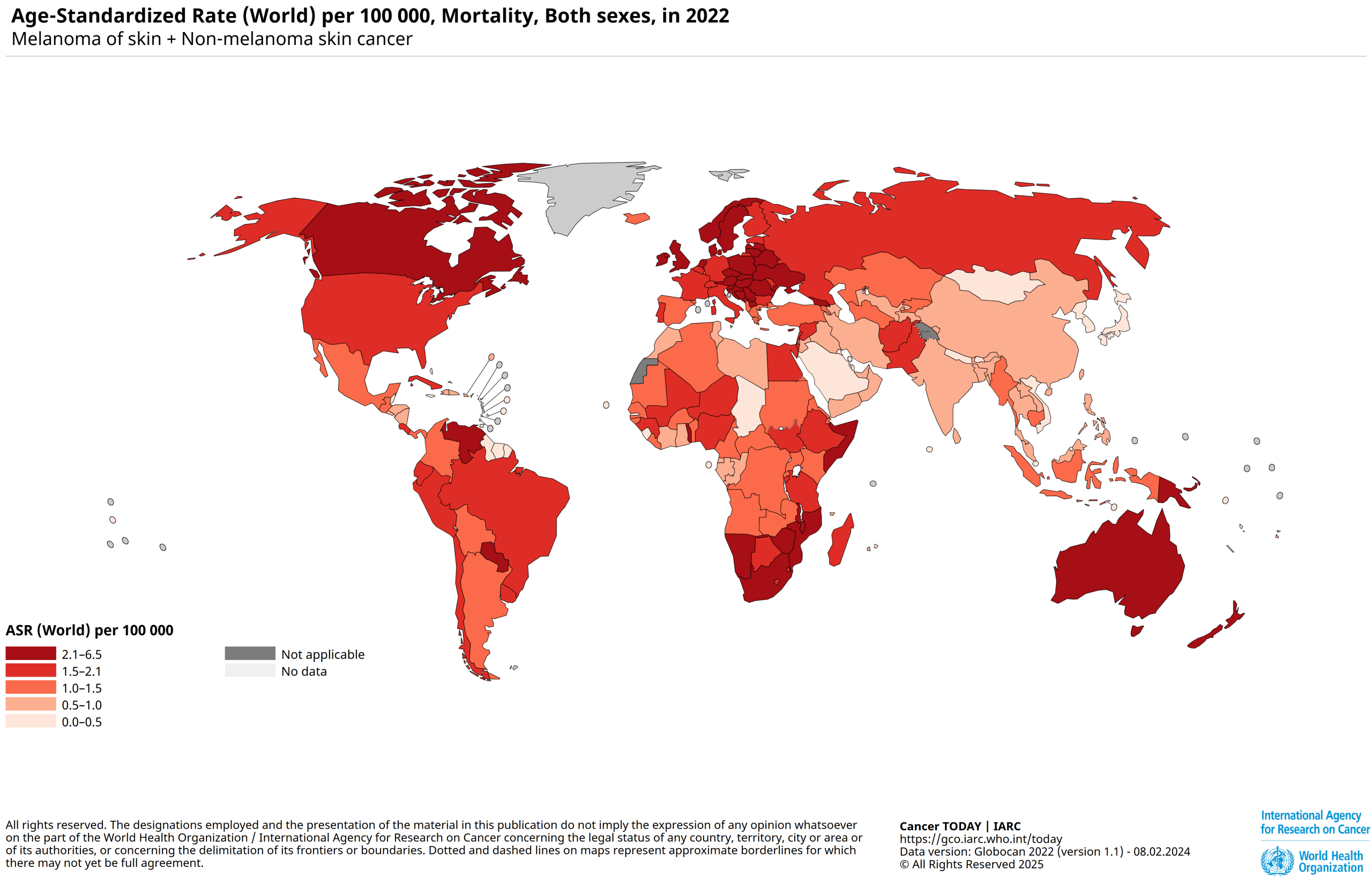
Global Skin Cancer Data
Exposure to ultraviolet (UV) radiation, whether natural or artificial, is the leading cause of skin cancer, including melanoma. According to the latest global estimates, over 75% of new melanoma cases are directly linked to UV radiation1.
In France, between 80,000 and 100,000 cases of skin cancer are diagnosed every year, making it the most common form of cancer. Melanoma cases alone have increased fivefold between 1990 and 2018, reaching approximately 15,500 new diagnoses annually. Although melanoma accounts for only about 10% of skin cancers, it is the most dangerous due to its high metastatic potential, a key factor in medical decision-making2.
Globally, over 1.5 million new skin cancer cases were reported in 2022, including 330,000 melanomas. That same year, nearly 60,000 deaths were attributed to the disease3.
With 330,042 cases diagnosed in 2022, non-melanoma skin cancer is the fifth most common cancer in Europe4.
In North America, skin cancer is also the most common, with over 5 million cases diagnosed each year5.
There can be a genetic component to melanoma6; people with a first-degree relative who has had melanoma are at significantly higher risk. However, sun-related behaviors are just as critical. Intense, intermittent UV exposure is known to trigger tumor development. On average, having just five sunburns in a lifetime can double one’s risk of developing melanoma.
Despite this concerning increase, therapeutic advances have yielded encouraging results: between 2010 and 2015, the age-standardized 5-year net survival rate for cutaneous melanoma reached 93%, reflecting increasingly effective care and treatment7.
Predictions for 2040
In 2020, around 325,000 new cases of cutaneous melanoma were diagnosed worldwide. If current trends continue, this number could rise to approximately 510,000 by 2040—an increase of nearly 57%8.
In 2021, considering all types of skin cancer combined (melanomas and non-melanoma carcinomas), the global incidence was estimated at 6.64 million cases, with an age-standardized incidence rate (ASIR) of 77.66 per 100,000 people. This rate could reach 101.73 by 2030, primarily driven by rising numbers of basal cells and squamous cell carcinomas9.
Regarding mortality, about 57,000 melanoma-related deaths were recorded in 2020. That figure is projected to climb to 96,000 by 2040—a 68% increase10.
Though melanoma accounts for a minority of skin cancer cases, it is responsible for most related deaths. In contrast, carcinomas represent most cases but are less fatal.
These projections underscore the urgent need to strengthen prevention strategies and ensure equitable access to care.
The Different Types of UV Rays
These figures serve as a wake-up call: better protection against UV rays is crucial—especially for children. Their stem cells are located closer to the skin’s surface than those of adults, making them more vulnerable to cancer-causing mutations. Direct sun exposure before the age of one is strongly discouraged.
On the beach, a basic umbrella blocks only 40–50% of UV rays; the rest reaches the skin through reflection or diffusion. Even on cloudy days—when many believe they’re safe from sun damage, up to 80% of UV radiation can still penetrate11.
Ultraviolet (UV) rays are a form of electromagnetic radiation emitted by the sun. They are invisible and exist in three forms: UVA, UVB, and UVC.
- UVA Rays: These penetrate deeply into the skin, causing premature aging and wrinkles. They also amplify the effects of UVB rays.
- UVB Rays: These rays damage the outer layer of the skin, leading to sunburn and playing a significant role in the development of skin cancer.
- UVC Rays: Largely absorbed by the Earth’s atmosphere, these rays do not reach the surface.
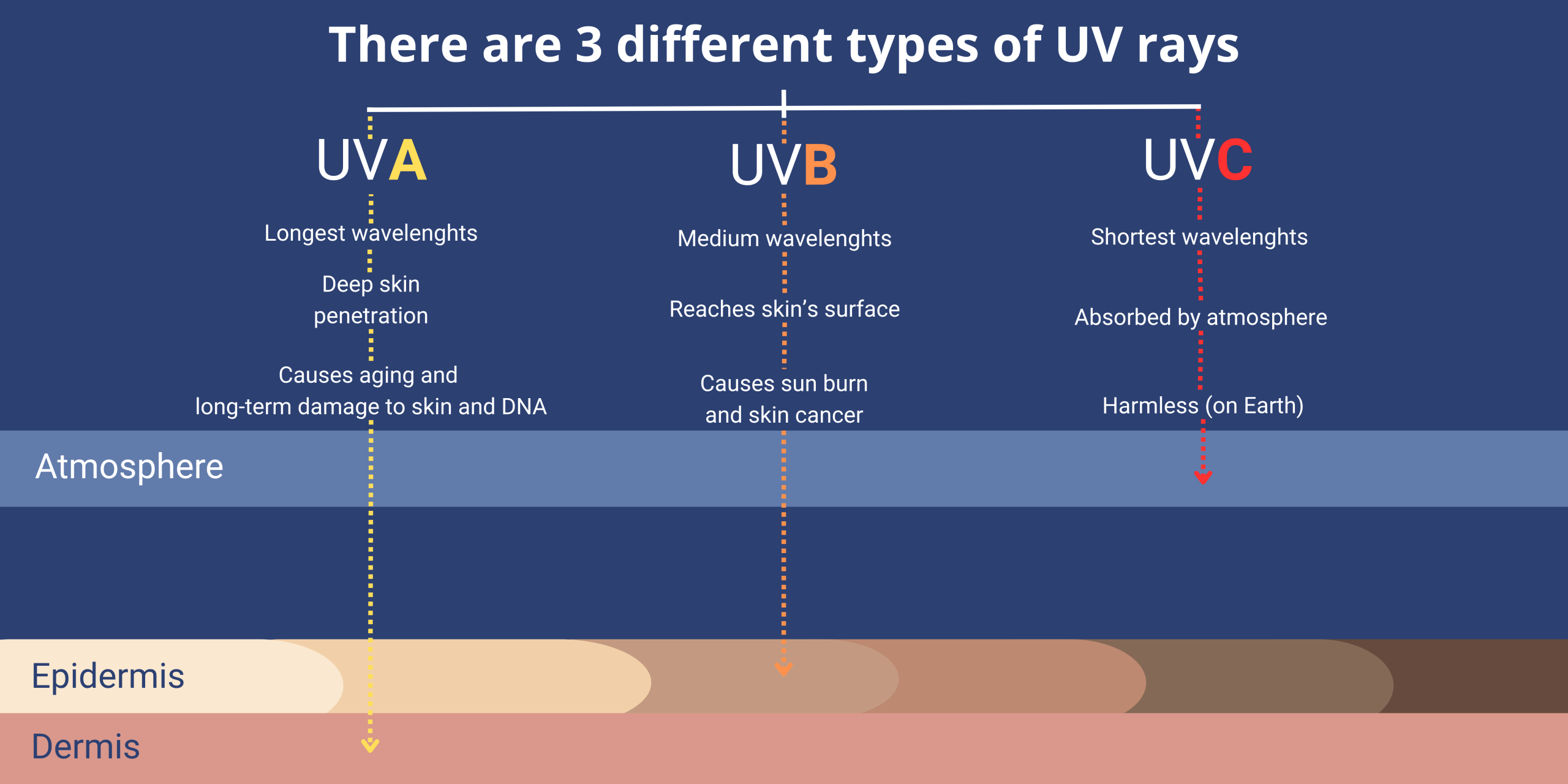
Since SPF only applies to UVB rays, it’s essential to choose a sunscreen that says “broad-spectrum” on the label—this indicates that the product helps protect against UVB and UVA rays. Both types of UV rays can damage your skin and contribute to skin cancer. As mentioned above, UVB rays are responsible for causing sunburns. UVA rays, on the other hand, are often referred to as “aging rays” because they can prematurely age your skin—resulting in fine lines, wrinkles, and discoloration. These rays may also damage your skin when you’re indoors.
Staying Protected
Unprotected skin can begin to suffer UV damage in as little as 15 minutes12.
For all these reasons, it’s essential to take the right precautions13.
– Apply SPF 50+ sun cream and reapply every 2 hours at least or more often if you go swimming or sweat.
– Stay in the shade as much as possible, typically between 12pm and 4pm.
– Wear light, long-sleeved clothing, a hat and sunglasses. For more fragile people, or in case of long exposure, wear clothing with a UPF (Ultraviolet Protection Factor).
– Check the day’s UV index to prepare yourself accordingly to it, you can find it on any app weather.

Cancer prevention has become one of the most critical public health challenges of the 21st century. Based on current scientific evidence, at least 40% of all cancer cases could be prevented through effective primary prevention14. Among those diagnosed, 50% undergo radiation treatments which still have limitations in their current form15.
Types of Skin Cancer

Squamous cell carcinoma (SCC)
Accounts for about 20% of all skin cancers. It typically appears on sun-exposed areas but can also develop on scars, chronic wounds, or old lesions. It is presented as thick, scaly, crusty, or bleeding patches. Fortunately, SCC becomes invasive in fewer than 1% of cases16.
Source: CBD Skin Cancer Clinic. (n.d.). Squamous Cell Carcinoma (SCC). https://cbdskincancer.com.au/skin-cancer/squamous-cell-carcinoma-scc/
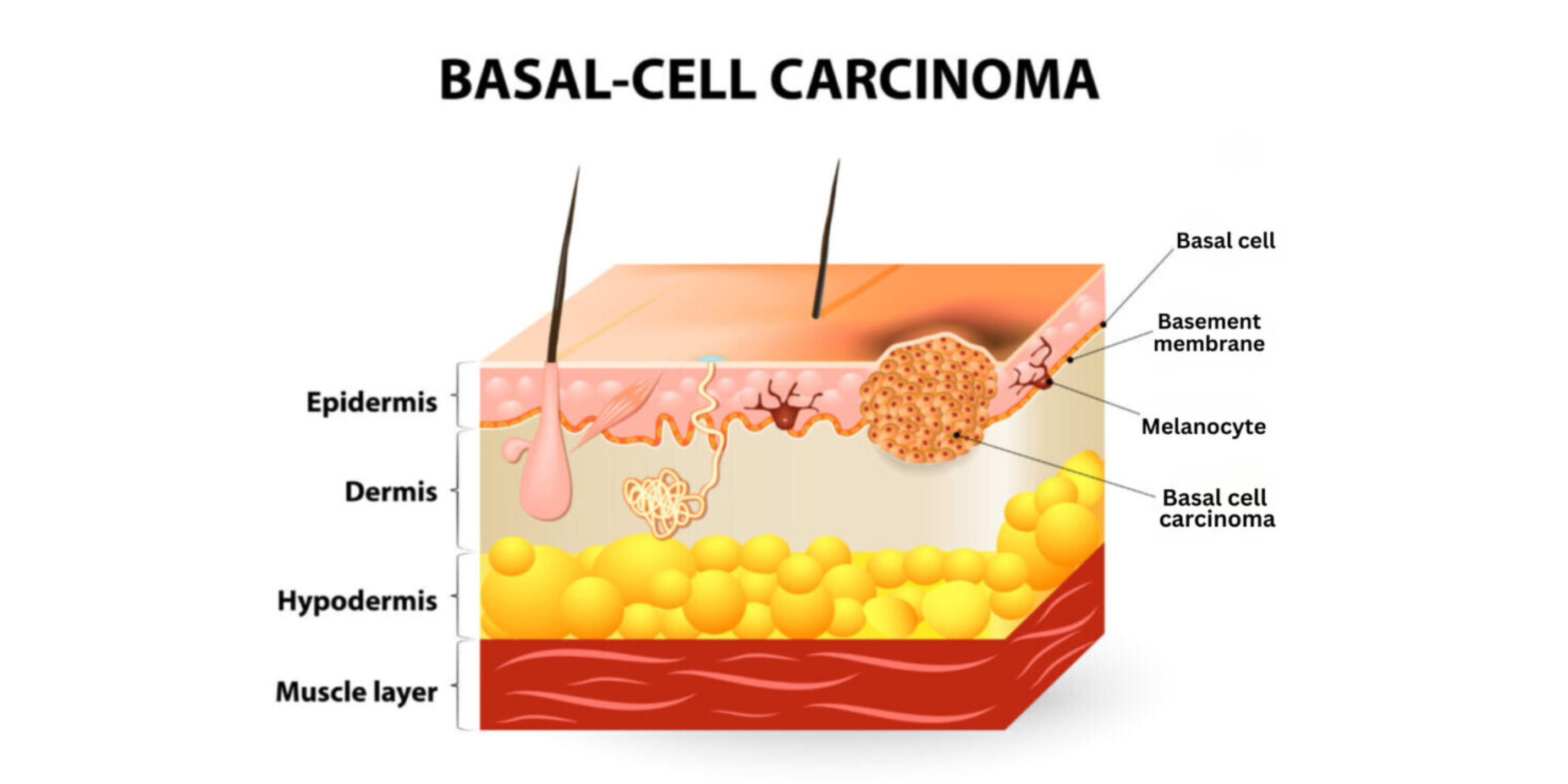
Basal Cell Carcinoma (BCC)
The most common form of skin cancer, representing around 70% of cases. It mainly affects fair-skinned individuals over the age of 50 and is most often found on the face. BCC usually appears as a persistent pink lesion. It does not metastasize, making it less dangerous16.
Source: CBD Skin Cancer Clinic. (n.d.). Basal Cell Carcinoma (BCC). https://cbdskincancer.com.au/skin-cancer/basal-cell-carcinoma-bcc/
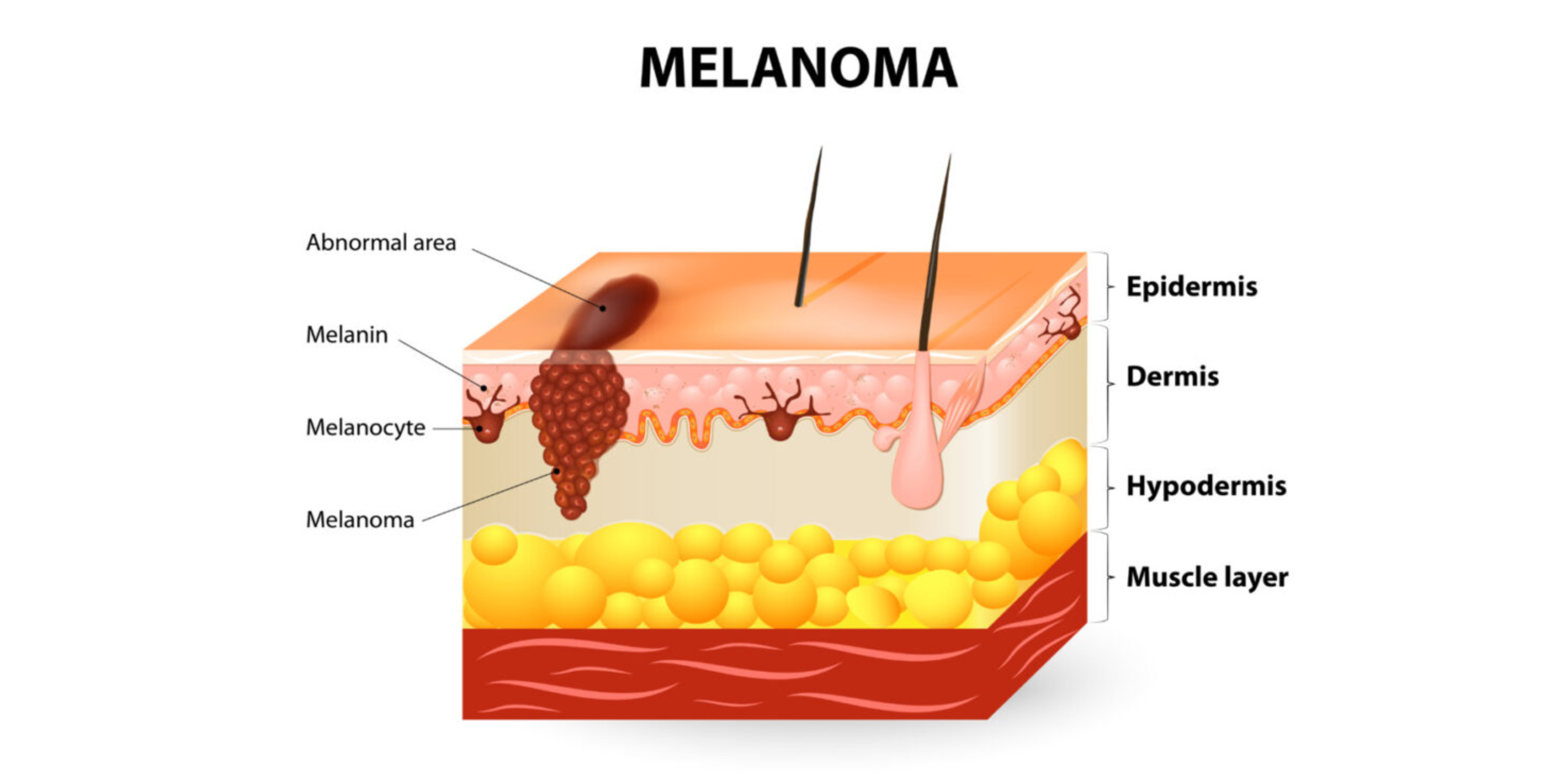
Types of Melanomas:
Melanomas are aggressive cancers because they spread (metastasize) quickly. There are primarily 4 major types of melanomas17:
Superficial Spreading Melanoma: This is the most common type of melanoma (70% of cases), often found on the lower limbs of women (legs and thighs) and the trunk of men (neck to hips). It is primarily linked to childhood sunburn, especially in fair-skinned individuals. The irregular brown or black spot develops horizontally and spreads outward for several years before penetrating deeper layers of the skin. Within just a few months, its volume and size increase.
Source: CBD Skin Cancer Clinic. (n.d.). Melanoma. https://cbdskincancer.com.au/skin-cancer/melanoma/
Dubreuil Melanoma (or Solar Melanoma): Also known as Lentigo Maligna, it typically appears in older individuals, especially on the face, ears, and arms, and accounts for 10 to 15% of melanomas. It appears as a large, flat, irregularly bordered brown or black spot (which should not be confused with age spots, which are often light or dark brown and found on the hands or face of seniors). It is associated with excessive sun exposure.
Acral Lentiginous Melanoma: This rare type of melanoma, affecting extremities, accounts for less than 5% of cases. It is more commonly observed in individuals with very dark skin or African descent (60% of melanoma cases in these individuals, compared to 5% in fair-skinned people). It usually develops on the palms, soles, or nails18.
Nodular Melanoma: This type appears as a simple “bump” that is brown-black, red, or bluish in color. Nodular melanoma should raise concern when it grows rapidly or bleeds with minimal friction. It forms a raised mass that protrudes from the skin’s surface (polypoid). It is the second most common melanoma, representing about 15% of cases. From the start, it grows deep, making early diagnosis challenging. As with many other cancers, the earlier the diagnosis, the better the prognosis.
Recognizing a Dangerous Skin Lesion

If any of the following points raise concern regarding one of your spots, do not hesitate to first contact your general practitioner, who will refer you to a specialist if necessary. In the case of a suspicious mole, the dermatologist will conduct a clinical examination, possibly supplemented by dermoscopy. If necessary, a biopsy will be performed to confirm or rule out the presence of melanoma.
Treatment depends on the diagnosis. In the case of melanoma, surgical excision is generally the first-line treatment. For more advanced cases, targeted therapies or immunotherapy may be considered.
Innovations and Artificial Intelligence
With a shortage of dermatologists and long wait times, new technologies paired with artificial intelligence are proving increasingly valuable for diagnosis.
Since October 2023, in Evreux, France, a three-meter-tall and five-meter-wide device equipped with 92 high-definition lenses can photograph a patient’s entire skin surface in one shot. The scanner produces a full-body map of lesions and moles19.
“The doctor can then, remotely, choose to magnify any suspicious mole for analysis”.
This type of technology could revolutionize early detection—critical for improving survival rates.
Researchers have developed AI algorithms20 capable of detecting skin cancers with 95% accuracy, surpassing the performance of many dermatologists. These tools could revolutionize screening by enabling faster, more accurate detection of malignant lesions.
After over 200 clinical studies and three years of research, an artificial intelligence system specialized in dermatology is now being tested in 14 countries, including France. Today, this cutting-edge technology can detect 96% of skin cancer cases with remarkable accuracy.
THERYQ’s Role in Advancing Radiation Oncology
This is where THERYQ comes in. We are committed to addressing a critical need: providing new treatment options, especially for patients who may not respond to conventional methods. Since the discovery of the FLASH effect, our mission has been to transform this technology into a clinically approved solution.
Sources
1. Arnold, M., de Vries, E., Whiteman, D. C., Jemal, A., Bray, F., Parkin, D. M., & Soerjomataram, I. (2018). Global burden of cutaneous melanoma attributable to ultraviolet radiation in 2012. International Journal of Cancer, 143(6), 1305–1314. Global burden of cutaneous melanoma attributable to ultraviolet radiation in 2012 – PubMed
2. Mathieu, O., Chaine, A., Benassarou, M., Combes, F., Debelmas, A., Lanciaux, S., Bertolus, C., & Bouaoud, J. (2024). Epidemiology of facial skin cancers managed in a French ambulatory surgical center. Journal of Stomatology, Oral and Maxillofacial Surgery, 125(3), Article 101726. Epidemiology of facial skin cancers managed in a French ambulatory surgical center – ScienceDirect
3. Melanoma Awareness Month 2022, by International Agency for Research on Cancer Melanoma Awareness Month 2022 – IARC
4. International Agency for Research on Cancer. (2022). Cancer Today: Pie chart – Cancer distribution. Global Cancer Observatory.
5. The Skin Cancer Foundation. (2019, July 26). Most Americans unaware of a widespread and potentially life-threatening skin cancer, according to Skin Cancer Foundation survey [Press release]. Most Americans Unaware of a Widespread and Potentially Life-Threatening Skin Cancer, According to Skin Cancer Foundation Survey
6. Ligue contre le cancer. (2021, June 29). Le soleil : savoir s’en protéger pour garder une peau en bonne santé. Le soleil : savoir s’en protéger pour garder une peau en bonne santé | Ligue contre le cancer
7. Epidemiology of skin cancers. Institut National du Cancer. Epidémiologie des cancers cutanés
8. International Agency for Research on Cancer. (2020). Global burden of cutaneous melanoma in 2020 and projections to 2040. Global Burden of Cutaneous Melanoma in 2020 and Projections to 2040 – PubMed
9. Zhou, L., Zhong, Y., Han, L., Xie, Y., & Wan, M. (2025). Global, regional, and national trends in the burden of melanoma and non‑melanoma skin cancer: Insights from the Global Burden of Disease Study 1990–2021. Scientific Reports. Global, regional, and national trends in the burden of melanoma and non-melanoma skin cancer: insights from the global burden of disease study 1990–2021 | Scientific Reports
10. Arnold, M., Singh, D., Laversanne, M., Vignat, J., Vaccarella, S., & Bray, F. (2022). Global burden of cutaneous melanoma in 2020 and projections to 2040. JAMA Dermatology, 158(5), 495–503. Global Burden of Cutaneous Melanoma in 2020 and Projections to 2040 – PubMed
11. Utrillas, M. P., Martínez‑Lozano, J. A., & Núñez, M. (2010). Ultraviolet radiation protection by a beach umbrella. Photochemistry and Photobiology, 86(2), 449–456. Ultraviolet Radiation Protection by a Beach Umbrella – Utrillas – 2010 – Photochemistry and Photobiology – Wiley Online Library
12. Hartford Hospital. (2018, May 23). Sun Can Damage Your Skin in 15 Minutes [News release]. Hartford HealthCare. Sun Can Damage Your Skin in 15 Minutes | Hartford Hospital | Hartford, CT
13. Ligue contre le cancer. (2023, August). Les cancers de la peau [PDF].
14. Wild, C. P., Espina, C., Bauld, L., Bonanni, B., Brenner, H., Brown, K., Dillner, J., Forman, D., Kampman, E., Nilbert, M., Steindorf, K., Storm, H., Vineis, P., Baumann, M., & Schüz, J. (2019). Cancer Prevention Europe. Molecular Oncology, 13(3), 528–534. Cancer Prevention Europe – PubMed
15. Lindner, J. (2025, May 1). Radiation therapy statistics: Market data report 2025. Worldmetrics. Radiation Therapy Statistics Statistics: Market Data Report 2025
16. American Cancer Society. (2024). Skin cancer facts & figures. Cancer Facts & Figures 2024
17. MédecinDirect. (2022, February 3). Mélanome : causes, symptômes, prévention et traitements. Mélanome : Causes, symptômes, prévention et traitements
18. Vidal. (2024, September 25). Mélanome : cancer de la peau. Mélanome (cancer de la peau) – symptômes, causes, traitements et prévention – VIDAL
19. Sciences et Avenir. (2024, June 10). Cancers de la peau : la technologie l’IA au service du dépistage Cancers de la peau: la technologie et l’IA au service du dépistage
20. La Provence. (2025, April 13). Une intelligence artificielle pour détecter les cancers de la peau aide les dermatologues à Villeneuve-lez-Avignon. Une intelligence artificielle pour détecter les cancers de la peau aide les dermatologues à Villeneuve-lez-Avignon