FLASH Radiotherapy
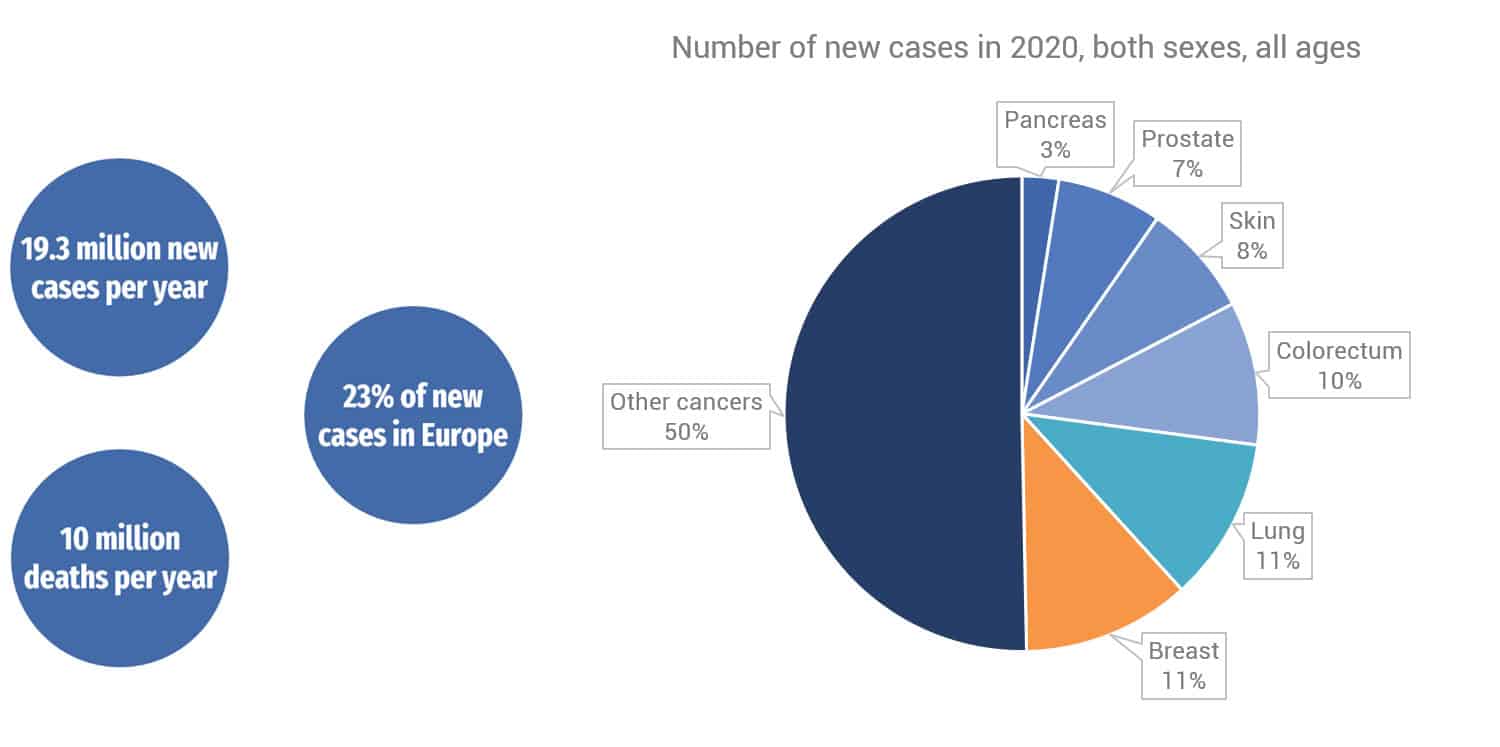
With more than 20 million new cancers and 10 million deaths per year, cancer is the second leading cause of death in the world1. Cancer care remains one of the most essential global health policy priority issues. Yet approximately a third of patients with solid tumors are still resistant to all cancer treatment modalities2. Together with surgery and chemotherapy or immunotherapy, radiotherapy is a major component of cancer care, recognized as one of the most cost-effective forms of cancer therapy. Based on radiotherapy indications, more than 50% of cancer patients receive at least one radiation treatment during the course of their disease, either alone or in combination with other treatment modalities3.
In the last decade, major advances in high precision treatment delivery and multimodal imaging allowed radiotherapy to be better tolerated, with an increased proportion of patients living longer, cancer-free or with durable cancer control, and with fewer side effects4.
|
FLASH Radiotherapy5 |
Conventional Radiotherapy6;7 |
|---|---|
| As few as one session | Between 5 and 40 sessions |
| Ultra-short irradiation time | Several minutes of irradiation time per session |
| Less toxicity to healthy tissues |
Side effects on healthy tissues, impacting patients’ quality of life |
| Lower direct and indirect cost of treatment | Higher cost of treatment |
| Fewer psychological symptoms for patients | Repetitive stress for patients |
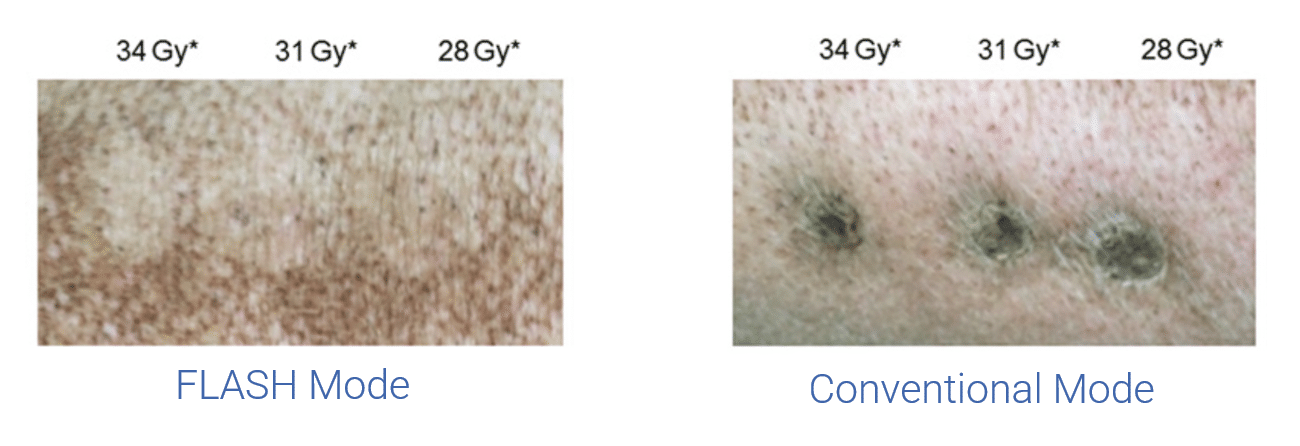
FLASH Radiotherapy consists of delivering ionizing radiation at an ultra-high dose rate, resulting in a delivery time of less than a tenth of a second. It has reproducibly shown a healthy tissue-sparing effect in several preclinical studies while still effectively destroying cancerous cells8;9;10.
Despite improvements, the efficiency of conventional radiotherapy is still limited by the radiation-induced side-effects on normal tissue surrounding the targeted area. FLASH-Radiotherapy is a revolutionary method which will significantly improve outcomes in cancer treatment.
FLASH radiation therapy has the potential to offer a more powerful and better tolerated treatment with several benefits over conventional radiotherapy and no equivalent today8;9;10:
- Patients could be treated in a single session as opposed to 5 to 40 sessions, for conventional radiotherapy, facilitating patient logistics and decreasing care cost in proportion to the number of sessions.
- Ultra-short duration of irradiation mitigates the problem of organ motion by conventional radiotherapy.
- A better tolerated treatment, i.e. fewer side effects, means better patient comfort and lesser side effects.
- For intra-operative applications, it could allow for a more efficient treatment with improved ergonomics and a much shorter irradiation time, facilitating the global operative logistics.
The FLASH effect has been studied since 2013 at CHUV in several preclinical studies (pig, zebrafish, mice, cats)11. Experiments on different species show that it has, for the same dose, the same destructive effect on the tumor as conventional radiotherapy, while sparing normal tissue, allowing a dose increase and a more efficient treatment.
It has also been tested on cat patients: the first FLASH radiotherapy tests were performed with 6 cats with epidermoid carcinoma of the nasal planum. The randomized testing has been done on a dozen cats in total. The tumors were treated successfully, and the protecting effect of FLASH was again demonstrated11.
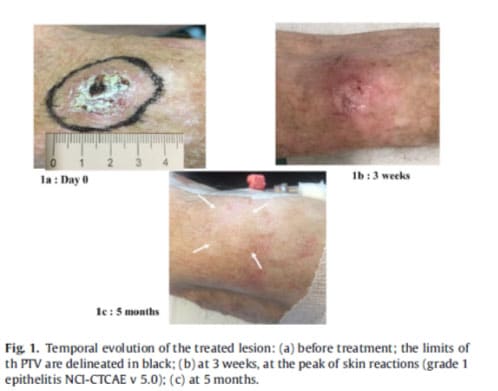
In 2019, a first patient was treated for a multi-resistant skin lymphoma: after having been treated over a hundred times with conventional radiotherapy systems, one lesion was treated using FLASH radiotherapy and it was a successful test9.
FLASH radiotherapy is a technique with significant potential in cancer treatment. By providing an efficient treatment in a fraction of a second, it is a quicker way to destroy tumors. The treatment is done in as little as a single session, as opposed to 5 to 40 sessions with conventional radiotherapy, which could allow patients to only come once. It has been shown to cause lesser side effects on healthy tissue, improving the quality of life for patients10. Finally, because of the reduction in the amount of treatment sessions and the expected efficiency of FLASH, direct and indirect costs are significantly reduced.
FLASH radiotherapy is a novel technique, delivering radiation at ultra-high dose rates in a fraction of a second. This modality is currently being studied and is not clinically available.
References
- Latest global cancer data: Cancer burden rises to 19.3 million new cases and 10.0 million cancer deaths in 2020. (n.d.). https://www.iarc.who.int/fr/news-events/latest-global-cancer-data-cancer-burden-rises-to-19-3-million-new-cases-and-10-0-million-cancer-deaths-in-2020/
- Busato, F., Khouzai, B. E., & Mognato, M. Biological mechanisms to reduce radioresistance and increase the efficacy of radiotherapy: state of the art. International Journal of Molecular Sciences, 23(18), 10211 (2022). https://doi.org/10.3390/ijms231810211
- How radiation therapy is used to treat cancer. (n.d.). American Cancer Society. https://www.cancer.org/cancer/managing-cancer/treatment-types/radiation/basics
- Chen, H. H., & Kuo, M. T. Improving radiotherapy in cancer treatment: Promises and challenges. Oncotarget, 8(37), 62742–62758 (2017). https://doi.org/10.18632/oncotarget.18409
- Favaudon, V., Caplier, L., Monceau, V., Pouzoulet, F., Sayarath, M., Fouillade, C., Poupon, M., Brito, I., Hupé, P., Bourhis, J., Hall, J., Fontaine, J., & Vozenin, M. Ultrahigh dose-rate FLASH irradiation increases the differential response between normal and tumor tissue in mice. Science Translational Medicine, 6(245) (2014). https://doi.org/10.1126/scitranslmed.3008973
- External Radiation Therapy. (n.d.). American Cancer Society. https://www.cancer.org/cancer/managing-cancer/treatment-types/radiation/external-beam-radiation-therapy.html
- Crompton, S. (2023, November 3). Ultra-high dose rate radiation: is FLASH the future? | Cancerworld Magazine. Cancerworld Magazine |. https://cancerworld.net/ultra-high-dose-rate-radiation-is-flash-the-future/
- Vozenin, M., Hendry, J., & Limoli, C. Biological benefits of ultra-high dose rate FLASH radiotherapy: Sleeping Beauty awoken. Clinical Oncology, 31(7), 407–415 (2019). https://doi.org/10.1016/j.clon.2019.04.001
- Bourhis, J., Sozzi, W. J., Jorge, P. G., Gaide, O., Bailat, C., Duclos, F., Patin, D., Ozsahin, M., Bochud, F., Germond, J., Moeckli, R., & Vozenin, M. Treatment of a first patient with FLASH-radiotherapy. Radiotherapy and Oncology, 139, 18–22 (2019). https://doi.org/10.1016/j.radonc.2019.06.019
- Schüler, E., Acharya, M., Montay‐Gruel, P., Loo, B. W., Vozenin, M., & Maxim, P. G. Ultra‐high dose rate electron beams and the FLASH effect: From preclinical evidence to a new radiotherapy paradigm. Medical Physics, 49(3), 2082–2095 (2022). https://doi.org/10.1002/mp.15442
- Vozenin, M. C., De Fornel, P., Petersson, K., Favaudon, V., Jaccard, M., Germond, J. F., Petit, B., Burki, M., Ferrand, G., Patin, D., Bouchaab, H., Ozsahin, M., Bochud, F., Bailat, C., Devauchelle, P., & Bourhis, J. The Advantage of FLASH Radiotherapy Confirmed in Mini-pig and Cat-cancer Patients. Clinical cancer research: an official journal of the American Association for Cancer Research, 25(1), 35–42 (2019). https://doi.org/10.1158/1078-0432.CCR-17-3375